How to maximize reimbursement in turbulent times
Skilled nursing facilities (SNFs) are experiencing monumental change. RUG-IV refinements have reoriented reimbursement for Medicare-covered services with significant funding reductions. There’s the focus on hospital readmissions within 30 days and how to prevent them. Never events that are deemed preventable have become the responsibility of the organization that is perceived to have caused them.
How does an organization adapt to these changes to capture market share, maximize reimbursement based on meeting patient needs and accurately capture all funding? At its core, optimal clinical outcomes—maximizing recovery of function quickly and minimizing complications—are among the performance dimensions being measured and are currently a key competitive driver in the market, determining winners and losers. In forecasting what the required competencies of organization leaders must be to successfully navigate the ever-changing environment one must cut through the chatter to distill the information and formulate key strategic objectives. Management competencies must build teams with clearly defined goals and organizational support enabling effective learning, performance measurement, target identification, integration of new skills and expanding goals based on successes.
 |
| Figure 1 |
As they emerge across the healthcare landscape, Accountable Care Organizations (ACOs) and Medicare replacement managed care contracts are examples of market forces that realign referral relationships and concentrate Medicare patients in fewer SNFs that demonstrate competency in managing medical conditions that deliver desired results and prevent costly mistakes.
While focusing on readmissions is a shift for acute care, this is not new in long-term care. Hospital transfers have always been a negative performance indicator. Lost days show up as a primary measure of performance in LTC financial statements. Lost revenue due to resident days missed while in the hospital has always been a conundrum for administration. It’s important to analyze root causes to identify preventable complications and implement earlier intervention while options are available in the SNF environment or identify necessary clinical skills that must be developed.
Hosts of approaches are available. For example, doctors must trust nursing assessment skills and suggested interventions. This occurs when physicians are an active part of the care team and administration aligns incentives that motivate doctors to look for solutions in the SNF, and hospital administrators cease to reward physicians that admit patients that can be managed outside the hospital. Physicians can act as teachers: expanding clinical knowledge of the nursing and therapy staff, improving their clinical skills and thereby enabling recognition of undesired changes in condition and intervening earlier. This illustrates the significance of managing all the variables influencing decisions that result in desired or avoidable outcomes and developing an implementation plan that addresses them.
What are the solutions that reverse the behaviors that lock systems in negative performance? First and foremost is building trust among team members; valuing the contribution by all regardless of their background and education. Everyone has something to contribute based on their perspective as long as they are committed to improving performance. Leadership must model its behavior for all staff, soliciting input and valuing participation in the process. As teams identify goals and strategies for implementation, leadership demonstrates its support by allocating resources for these activities.
Administration participates in pilots, reinforcing the importance for others whose instinctive response is that they do not have the time in addition to their regular duties as well as celebrating success as a team and an organization. The key is genuine interest in the people and their journey. An illustration of this is the organizational approach employed in the assessment, care planning, monitoring process and preparation for the RUG-IV changes in the SNF I administered, Ballard Rehabilitation in Des Plaines, Ill.
CASE STUDY: BALLARD REHABILITATION
While serving at Ballard Rehabilitation, my team assembled representation from all disciplines that provide care and have a corresponding section on the MDS. We conducted training in the MDS and RUGs along with software that enabled all to independently complete their respective sections in addition to analytical software to identify opportunities to capture all appropriate reimbursement. We used two analytics programs which helped us identify specific patient information issues and make corrections or review the care provided to maximize reimbursement. An information flow was created that enabled the teams to share patient information that impacted care and reimbursement targets.
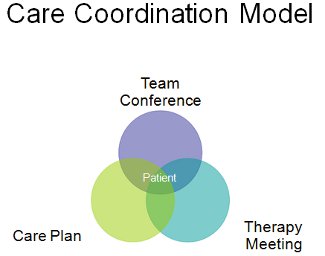
The conceptual model as illustrated in figure 1 reveals a patient-centric care coordination system and how each team’s work product contributed to the delivery of timely and effective care along with corresponding funding. The transitional patients are all in an intense treatment program which includes both rehabilitation and medical populations. This team meets weekly and includes a physician and case manager from an insurer that has a large volume of patients as well as a nurse practitioner from a medical group. The meeting is organized by payor group or caseload to minimize the time for outsider participants. Volumes and time frames are provided for planning purposes.
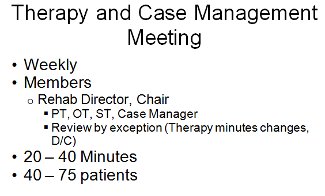
The patients with changes in condition or treatments which could be a result of improvements or decline as well as those requiring discharge are reviewed weekly at the therapy and case management meeting illustrated in figure 2. Its focus is on treatment goals and capturing appropriate reimbursement. The patients reviewed are by exception rather than caseload to maximize productivity. Long-term residents are reviewed in the quarterly care plan meeting. This is where restorative programs are discussed and whether any residents can benefit from more intense treatment in therapy or medical programs.
 |
| Figure 2 |
All of these meetings are at the core of the organization’s ability to effectively manage and coordinate care and services, which enables the organization to capture the maximum available reimbursement regardless of payer source. Success of this model is dependent on the team’s ability to work collaboratively and share the pertinent information on each patient. All members must be prepared and understand the key pieces of information that their peers need to meet patients’ care goals and enable the organization’s ability to support the RUG scores or insurance levels and bill appropriately. In light of the financial pressure from Medicare cuts and competitive pressure to capture market share, organizations must demonstrate their ability to hit care and financial targets to remain profitable. These are accomplished within a management system that delivers breakthrough performance improvements.
Eli Pick, CNHA, CAS, FACHCA, is President of Post Acute Innovations. He serves on the editorial advisory board of Long-Term Living. Contact him at epick@postaccutein.com.
I Advance Senior Care is the industry-leading source for practical, in-depth, business-building, and resident care information for owners, executives, administrators, and directors of nursing at assisted living communities, skilled nursing facilities, post-acute facilities, and continuing care retirement communities. The I Advance Senior Care editorial team and industry experts provide market analysis, strategic direction, policy commentary, clinical best-practices, business management, and technology breakthroughs.
I Advance Senior Care is part of the Institute for the Advancement of Senior Care and published by Plain-English Health Care.
Related Articles
Topics: Articles , Facility management , Leadership











