Developing a therapeutic recreation dementia program
At a glance…
Through dedicated staff training, assembling these “pieces of the puzzle” yielded many facility-wide benefits.
Village Nursing Home has seen dramatic success in its project to enrich the abilities of staff interacting with residents with dementia-a project named “Pieces of the Puzzle.” The project has two objectives: (1) truly empowering certified nursing assistants (CNAs) to support a person-centered care model; and (2) providing these empowered CNAs with the best therapeutic recreation tools, in accordance with the American Therapeutic Recreation Association’s (ATRA) Dementia Guidelines.
At the time of project development, Village Nursing Home understood that caregiver decision making and authority composed the foundation of any efforts to improve quality of care and quality of life for its residents. Among the Pioneer Network facilities that have created person-centered care environments, those who have seen positive outcomes in resident satisfaction and other quality-of-life measures-including Chase Memorial (the first Eden Alternative home), Providence Mount Saint Vincent, and the Wellspring facilities-have been those who have “empowered” the frontline caregivers. Almost all facilities that have empowered their CNAs and created person-centered cultures of care have also seen dramatic decreases in staff stress levels, which studies have linked to resident abuse and neglect. Furthermore, Drs. Reinhard and Stone, in their formal evaluation of the Wellspring Model, noted a link between quality-of-care measures and CNA empowerment.1 Clearly, person-centered care through caregiver empowerment is a “best practice” work environment intervention that improves the health and quality of life for residents.
Yet, the Village Nursing Home project was unique because it combined person-centered care efforts with a “toolbox” of evidence-based dementia recreation methods and the ability to personalize activities. Therapeutic recreation provides many health and quality-of-life benefits for nursing home residents, particularly those with dementia. More than simple diversion, purposeful and meaningful activities will improve mental status and functioning. In fact, study after study has shown that nursing home residents with cognitive impairments who receive recreation therapy demonstrate significantly improved depression levels, increased activity and alertness levels, and lowered fall rates. Yet, in most nursing homes, many residents access activity programs only occasionally, and those programs are not always suited to an individual’s preferences or even functional level.
The Pieces of the Puzzle project made on-unit, individualized activities the responsibility of every CNA. Drawing on best practices and the Dementia Guidelines, CNAs first learned a bit about each of their residents and then made meaningful activities ubiquitous on the unit. For example, “personal [workstations] activities” that are designed with the resident’s past life story/occupation in mind have been very successful; these can include a mock office area, baby care items with lifelike baby dolls, sheets or linens for folding, or simple tools. Residents are able to wander in and out of the activity area during the day, engaging in individual, meaningful activities that allow them to explore and manipulate.
By integrating therapeutic recreation planning and activities into improved caregiving responsibilities and into the caregiver-resident relationship, we anticipated the following benefits:
lower levels of agitation
lower levels of depression
increased engagement and socialization
Methods
The Pieces of the Puzzle project sequenced the two interventions, with the first four months of the project concentrating on building a person-centered care environment. This was accomplished by:
selecting staff who expressed a preference to work with residents with dementia;
implementing consistent assignment of CNAs to individual residents (as the consistent assignment of caregivers to residents enables CNAs to gain important insights into each person) and;
training the CNAs in communication and problem solving, through working with the Paraprofessional Healthcare Institute (PHI) and their Pioneer Network training modules.
However, we understood that training the CNAs was not sufficient in itself to support such a dramatic change in their responsibility and authority-changes in their supervisory relationships were also required. Therefore, the dementia unit’s nurses, social workers, therapeutic recreation staff, and other supervisors were trained by PHI in “Coaching-Supervision.” This method of supervision focuses on relationship-building and on the role of supervisors in supporting further development of problem-solving skills on the part of line staff.
The final component of building CNA-empowerment was the establishment of a biweekly support group for the unit’s CNAs. Dubbed “post-training discussion groups,” the CNAs met to discuss their new roles and to share concerns and ideas, and these were also used as “booster sessions” for the training material.
Once the CNAs and supervisory staff became used to their new interactions and had some practice in their new decision-making and caregiving responsibilities, the CNAs on the unit began their training in the ATRA Dementia Practice Guidelines. The two-day training sessions involved: a review of where to find information about the resident and his/her behaviors; a review of the most effective interventions for particular behaviors and interests, and a discussion of the theory behind their effect; a discussion of other ideas CNAs might have for effective recreation interventions; and activity planning practice for the unit’s residents.
The content of these trainings-and CNAs’ experiences with trying and doing different activities with the residents-were also incorporated into the weekly CNA Discussion Group.
Results
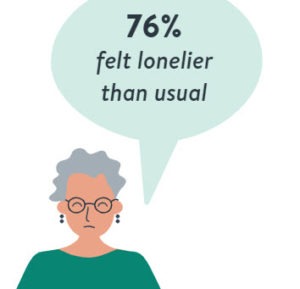
The Pieces of the Puzzle project has achieved a great deal of success, including some crucial yet unanticipated benefits. First, the dementia unit’s residents did indeed show improvement in their moods. Upon review of mood scale items from the Minimum Data Set scores [identified in E1a, E1c, E1f, E1g, E1n, E1m, K4c, E2], the number of patients on this unit triggering for mood problems steadily declined, dropping by 67% during and after the intervention (see figure).
Not only does this improvement in mood show up in the MDS, but staff and family have observed improvements in residents’ affective behavior, such as decreased agitation and increased social interaction. Consider these examples:
Mr. C would act out while receiving morning care or whenever he was to shower. As a result of the training, staff learned from a visitor about Mr. C’s interest in jazz. Staff played jazz music for him and discussed the artists or had him join in on the rhythms and beats. Mr. C is now distracted and comfortable with the tasks being performed.
Mr. S would become randomly agitated while sitting idle. One staff member, picking up on the knowledge that his past occupation was theater production and makeup, provided him with a female mannequin head, makeup, and hair accessories. Mr. S expressed pleasure in working with the mannequin head to create various hair designs, at times carrying on a conversation with the mannequin.
Ms. H, a Cantonese-speaking resident, would sit quietly and participate in no activities beyond “people watching.” After the training, a CNA offered her a ball of yarn and some needles and showed her how to crochet. At their next visit, the family was pleasantly surprised to see her sitting at a table working diligently on her creation. Once another staff member noticed that Ms. H liked to work with her hands, she found a Chinese writing kit which she provided for her use; Ms. H now alternates from yarn work to writing, and is actively engaged throughout the day.
The Pieces of the Puzzle project resulted in other important improvements. First, since implementing the project, we have noticed that the rate of falls on the unit has decreased. In fact, the data revealed a significant decrease in the number of falls from this unit, dropping by 53.3% in one year alone.
Another important outcome is the impact on staff satisfaction. While our intent was to improve the residents’ quality of life directly, staff satisfaction is a vital component to that and indirectly improves the residents’ experiences. We attribute the facility’s staff satisfaction improvements to the dementia project because of the feedback that participating staff have provided-for example:
“The training created a cohesive team through communication skills. As it turned out, we don’t need to always look to change the behavior in the resident, but can look to change staff behavior in response to the resident.” (Supervisor)
“We learned how to reapproach and redirect our residents. We learned how ask open ended questions of our coworkers so that we could have better support and cooperation.” (CNA)
The impact on staff satisfaction can also be seen in the 0% turnover among CNAs on the Dementia Unit since the project began three years ago. While Village Nursing Home has always experienced low CNA turnover, averaging 12% annually-compared to statewide averages of 42% and national averages of 71%-having no resignations or terminations for three consecutive years is a significant achievement.
Conclusions
The project has achieved benefits beyond our initial expectations-benefits that can easily be replicated in other facilities. As a result of Pieces of the Puzzle, falls on the unit dramatically decreased, staff satisfaction appears to have increased, and CNA turnover has disappeared. All these benefits are a result of improving the teamwork on the unit, a team now driven to provide the residents with meaningful daily interactions. Overall, the combination of dementia education and new ways of problem solving empowered the staff to develop creative interventions to everyday challenges.
Visit www.villagecare.org/dementiatraining to watch Village Nursing Home staff discuss their therapeutic recreation dementia program.
Allison Silvers is Director of Strategic Initiatives; Aimee Montgomery Wilson was, at the time of writing, Director of Therapeutic Recreation (and is currently a certified coach and consultant at Ripple Coaching and Consulting); and Gregory Westgate oversees Therapeutic Recreation at Village Nursing Home, New York, New York. For more information, contact Gregory Westgate at
gregW@vcny.org or, for detailed information on the program, visit
https://vcny.org/dementiatraining.
To send your comments to the editor, e-mail mhrehocik@iadvanceseniorcare.com.
Reference
- Promoting quality in nursing homes: The Wellspring model. Reinhard, Susan and Stone, Robyn. January 2001. The Commonwealth Fund.
Long-Term Living 2010 June;59(6):42-45
I Advance Senior Care is the industry-leading source for practical, in-depth, business-building, and resident care information for owners, executives, administrators, and directors of nursing at assisted living communities, skilled nursing facilities, post-acute facilities, and continuing care retirement communities. The I Advance Senior Care editorial team and industry experts provide market analysis, strategic direction, policy commentary, clinical best-practices, business management, and technology breakthroughs.
I Advance Senior Care is part of the Institute for the Advancement of Senior Care and published by Plain-English Health Care.
Related Articles
Topics: Alzheimer's/Dementia , Articles