Rethinking Caregiving in America: A Framework for Growth and Sustainability
The case for supporting family caregivers as an integral part of the care team, with examples of innovation from Geisinger, Rush University Medical Center, and Duke University School of Nursing.
Almost 48 million adults in the U.S. care for another family member — an estimate the Centers for Disease Control and Prevention (CDC) closely tracks and now calls “a public health issue” for millions of Americans receiving care, as well as those providing the care.
Understanding the Challenge
The significance of the caregiving market to the health care industry — and the economy in general — can’t be overstated. Research conducted by AARP estimates the unpaid work provided by family caregivers at 36 billion hours or $600 billion, more than all the out-of-pocket health care spending in 2021.
Approximately 58 million adults are 65 or older today. That’s about 17 percent of the population, a number expected to grow to 22 percent by 2040. Without question, the aging of America will continue to have a large impact on our society — from the economy in general, to the health care industry specifically. But volunteer caregiving as an industry remains a largely fragmented and disjointed ecosystem.
While some health systems and community organizations offer basic education and limited resources to caregivers, it’s not an area of high strategic priority or significant investment for most health care executives or industry leaders.
But given industry trends such as the rising costs in health care delivery, the shortages of health care professionals (especially in rural areas), the growing demand for chronic-care management, and the requirements to shift more care into the home, there are good reasons for health care leaders to rethink the importance of this cohort and find ways to leverage their presence in more impactful ways.
Here, we take a quick look at recent initiatives led by the federal government, share some programs developed by forward-thinking health systems, and propose a framework based on technology that health care executives can use to reimagine the role of caregivers.
Growing Urgency and New Legislation
The Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act of 2017 called for the establishment of the Family Caregiving Advisory Council to advise and provide recommendations, including identifying best practices, to the Secretary of the U.S. Department of Health and Human Services (HHS) on recognizing and supporting family caregivers.
A recent report includes 26 recommendations collected through a wide range of industry research and listening sessions conducted between 2019 and 2021. One of five priority areas identified in the report calls for increased emphasis on integrating the caregiver into processes and systems from which they have been traditionally excluded.
In April 2023, the White House issued an Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers. While the order covers a wide range of both childcare and senior care issues, some significant elements focus on the latter, including:
- Innovative new health care payment and service delivery models focused on dementia care that would include family caregiver support.
- Investing in better ways to evaluate and set expectations for family caregivers in the Acute Hospital Care at Home program.
- Ensuring that hospitals actively involve family caregivers in the discharge planning process.
- Promoting best practices such as partnerships with community-based organizations and using resources from the Administration for Community Living and the Agency for Healthcare Research and Quality.
It’s too early to know what impact recent regulation and the associated recommendations to entities like HHS and CMS will have on health systems and payers, but recent trends suggest serious recognition by leading advocacy groups and the government that investing in and supporting unpaid caregivers is an important initiative.
“The need for caregiving support tied to individual health systems and entire communities is only growing and will require better scaling and efficiency if the health care industry is going to capitalize on leveraging caregiving to manage costs, improve quality, and impact the health care experience.”
Clearly, payers and providers are looking at new incentives for investing in more infrastructure and resources to advocate on behalf of, integrate in a more meaningful way, and provide more ongoing support to caregivers and their families. And in some cases, there may be penalties for not doing more.
How should health care leaders approach the caregiving industry, given its inherent lack of structure and organization?
Innovative Caregiving Programs
For health care organizations that already have caregiving resources and programs in place today, now is the time to evaluate those initiatives, and look for ways to aggressively expand on what works. Others can follow their lead.
Here are some examples of innovation:
- Geisinger has had great success with its LIFE Geisinger program to help seniors live independently in the community, reducing costs for participants by half since the program was introduced.
- Rush University Medical Center piloted a dedicated Caregiver Intervention program in 2020 that prioritizes family caregivers though both system-level changes and direct caregiver interventions.
- Planetree International has pioneered new caregiver programs and practices for its members, including pioneering language that reflects how “everyone is a caregiver” as part of its person-centered care philosophy and approaches.
- Duke University School of Nursing has created The Duke Elder Family/Caregiver Training (DEFT) Center, a new training and education program around everything from incorporating family caregivers into post-discharge care to addressing health inequity and social determinants of health.
Leveraging a Technology Framework
Within the technology industry are several key business strategies — specifically the concepts of platforming, scaling, and network effects — that health care executives can use to reimagine the role of caregivers from a somewhat disjointed and less efficient presence, to one that is an even more powerful, resourced, and impactful movement, and that generates even greater value for those receiving care as well as the health care industry itself.
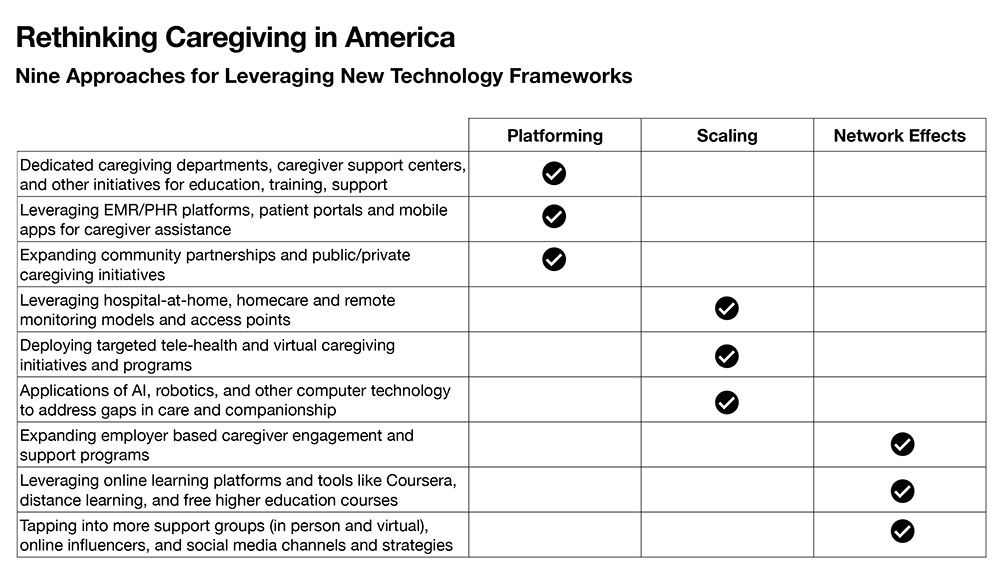
Platforming
In the tech industry, platforming refers to the use of software or technology to create a foundation or infrastructure that allows other applications or services to be built on top of it. Think of computer operating systems, social networks, gaming systems, etc.
In many respects, caregiving lacks that foundation because it is so individual in nature — every caregiver and family member experiencing the journey on their own, with little training, few resources, and significant isolation.
Even experienced health care professionals who become family caregivers often cite the same steep learning curves and frustrations navigating the “health care system” experienced by others.
By finding ways to platform caregiving, the health care industry would create a stronger foundation for caregivers that delivers more efficiency and success, and allows for more entities to connect and support caregiving in the community.
Some examples might include:
- Creating formal caregiving functions or departments within a health system or health plan.
- Leveraging existing electronic and personal health record systems to meet the unique needs of caregivers and family members.
- Forming more robust and innovative community partnerships to address the needs of caregivers.
Scaling
Scaling refers to the ability of a system to handle an increasing amount of traffic or work without sacrificing performance or stability. The concept is immediately applicable to caregiving, at both the individual family and community or industry-wide levels.
Individual caregiving demands often follow a common and predicable trajectory — often starting out slowly with nominal requirements of time and resources, but growing over time, sometimes even accelerating exponentially in later stages.
Similarly, the need for caregiving support tied to individual health systems and entire communities is only growing and will require better scaling and efficiency if the health care industry is to capitalize on leveraging caregiving to manage costs, improve quality, and impact the health care experience.
Scaling is an important concept that enables businesses to grow their operations, address market dynamics, and overcome limitations that might otherwise hinder success.
Some examples of scaling within the caregiver ecosystem might include:
- Leveraging hospital-at-home, homecare, and remote monitoring models.
- Using telehealth and virtual caregiving initiatives.
- Leveraging AI and robotics in ways Germany, Japan, and other countries have been able to do.
Network Effect
The network effect in technology and business refers to the idea that the more people or devices use a particular service, the more valuable it becomes for everyone involved, and the more it attracts others to the same platform or network.
It’s all about the power of community and impact where the value grows exponentially as more and more people connect. Social media networks like Facebook and TikTok may be the ultimate example of highly leveraged and successful network effects.
Some examples of creating a network effect within caregiving might involve:
- More aggressive employer-based caregiver engagement and support programs. Employers are impacted directly from the productivity and absenteeism due to caregiving demands of workers.
- Leveraging online learning platforms and tools like Coursera, distance learning, and free higher education courses.
- Expanding and tapping into support groups, influencers, and social media channels more aggressively.
These strategies, borrowed from the tech and startup industries, are just a few examples of how caregiving could be expanded and made more integral to the health care industry. And while not meant to be an exhaustive list of ideas or solutions, it may provide an innovative approach to ensuring the caregiving market is robust, supported, and able to meet growing demands of the health care industry and our society’s aging population.

Daniel Fell is senior vice president, Healthcare at BVK. He serves on the eHealthcare Strategy & Trends Editorial Advisory Board.
Related Articles
Topics: Featured Articles











