Stroke? Think FAST
It seemed like a routine day when my friend Renee (a pseudonym) went to visit her grandmother in the skilled nursing facility (SNF) where she lived—until Renee arrived at her grandmother’s room. She found the elderly woman unable to speak and rushed to the nurses’ station to relay the information to an aide. Having some background in health matters, Renee knew that speech difficulties can be a sign of stroke.
“Yeah, she was pretending she couldn’t talk when I was in there a little while ago,” the aide responded. The aide said she was about to take her break, so Renee called for other assistance.
My friend and I, perhaps naively, were astonished by the healthcare knowledge and sense of urgency lacking in this scenario. According to Laura Beving of the National Stroke Association (NSA), however, such occurrences are not rare.
“What you’re saying does not come as a surprise to me, unfortunately,” she said after I relayed the story. “The staff turnover in long-term care [LTC] facilities is crazy, so just training people to do what they have to do is huge. Doing additional training about stroke does not necessarily always happen the way it needs to.”
Beving, manager of stroke survivor and caregiver education and outreach for NSA, said that awareness of stroke signs, symptoms and treatments among those working in healthcare settings is important for three reasons:
- Time matters. A quick response can lessen damage and disability.
- Risk of repeat. Those who have had a stroke are five times more likely to have another one. It’s vital, therefore, to pay attention to modifiable risk factors such as hypertension, atrial fibrillation, high cholesterol, diabetes, cigarette smoking, alcohol use and sleep apnea and other sleep disturbances. “Sixty-five percent of people who have had a stroke suffer from some kind of sleep apnea following the stroke, and it’s also a contributing factor to people having strokes,” Beving said. Such risk factors, she added, “don’t necessarily get evaluated and treated, and they have serious implications on both recurrent stroke and also on recovery.”
- Rehab challenges. Rehabilitation can help address the effects of stroke, but stroke affects the rehabilitation process because it causes changes in emotion, communication and cognition as well as physical changes. Eighty percent of people experience incontinence after a stroke, which can lead to skin breakdowns and infections, and 75 percent are depressed due to changes in the brain and in their overall functioning, Beving said. Swallowing difficulties resulting from stroke can lead to aspiration pneumonia, and thirst receptor issues can cause people to become dehydrated and have urinary tract infections. Hemiparalysis can lead to spasticity (muscle contractions), affecting people’s ability to control their movements and care for themselves.
Learning more
Continuing education requirements for healthcare professionals generally are determined at the state level, Beving said, and they frequently apply only to administrators and sometimes nurses. The required annual hours, often 12, aren’t necessarily related to any specific health concern. That doesn’t mean that employers and employees can’t pursue education on their own, however.
The Commission on the Accreditation of Rehabilitation Facilities has established specific quality standards that apply to the stroke rehabilitation continuum. The Neuromotor Recovery and Rehabilitation Laboratory offers a certified stroke rehabilitation specialist program for licensed occupational and physical therapists, the exam of which is facilitated through the NSA. And the Association of Rehabilitation Nurses offers education, as do other professional societies for doctors, nurses and others.
The NSA offers continuing education as well as information on its website, www.stroke.org. Materials developed for healthcare professionals as well as for patients would benefit those who want to learn more about stroke, Beving said.
Beyond its website, Beving said the stroke association is happy to answer questions directly. “We’ve got a really friendly and helpful staff, so if people have questions, feel free to email and call,” she said. Find contact information at the aforementioned website.
 Beving added that communities across the spectrum of long-term care can take other action to ensure that all employees—not just those directly involved in the delivery of care—as well as residents and their families can recognize stroke signs and symptoms and understand the importance of early treatment:
Beving added that communities across the spectrum of long-term care can take other action to ensure that all employees—not just those directly involved in the delivery of care—as well as residents and their families can recognize stroke signs and symptoms and understand the importance of early treatment:
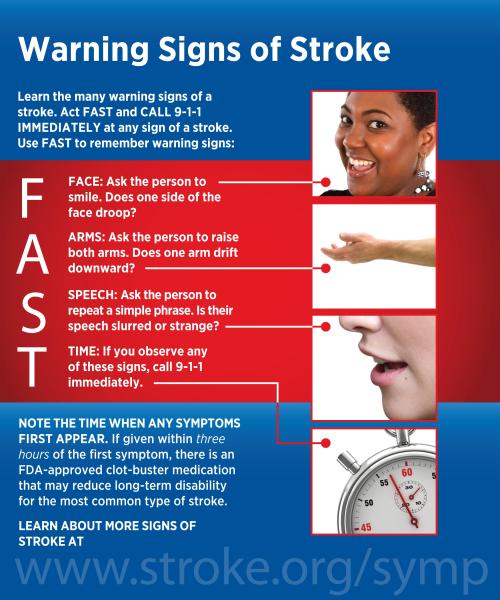
- Place posters, magnets and placards describing the FAST (Face, Arms, Speech, Time; see graphic) technique in elevators, employee break rooms and common areas. A downloadable wallet card is available at the link in the previous sentence.
- Conduct periodic in-service programs for staff.
The most important message to communicate to everyone is that stroke is an emergency, Beving said. “Don’t hesitate. Call 911,” she added. That’s important because an ischemic stroke often can be treated with tissue plasminogen activator, or t-PA, to dissolve the clot, “but there are time limits on it, and the faster you get it, the better—the less damage there is,” Beving said.
“ ‘Time is brain’ is something you’ll hear over and over again,” Beving said. “Even if someone is in [an LTC] facility, having them lose what they’ve got doesn’t serve anyone’s purposes.”
May is National Stroke Awareness Month, so it’s a great time to start the education process in your community.
As for the SNF where Renee’s late grandmother lived? Renee called the administrator, but he did not return her call. Sometime later, she spoke with the assistant director of nursing, not naming her grandmother or the aide. “I didn’t want to get anyone in trouble,” Renee said. “It just sounded like a good opportunity for additional training.”
Access all blogs by this author.
I Advance Senior Care is the industry-leading source for practical, in-depth, business-building, and resident care information for owners, executives, administrators, and directors of nursing at assisted living communities, skilled nursing facilities, post-acute facilities, and continuing care retirement communities. The I Advance Senior Care editorial team and industry experts provide market analysis, strategic direction, policy commentary, clinical best-practices, business management, and technology breakthroughs.
I Advance Senior Care is part of the Institute for the Advancement of Senior Care and published by Plain-English Health Care.
Related Articles
Topics: Clinical , Executive Leadership , Rehabilitation











